SHEIKH FAZILATUNNESSA MUJIB MEMORIAL
KPJ SPECIALIZED HOSPITAL
0244077031.
0244077030.
SHEIKH FAZILATUNNESSA MUJIB MEMORIAL
KPJ SPECIALIZED HOSPITAL
JOURNAL ARTICLE
Vol 1 Issue1 January 2023 Share Share
Worldwide, Primary liver malignancy is the sixth most common cancer. Hepatocellular carcinoma (HCC) comprises 90% of them.¹, ² It is the fifth most common cancer in men and the ninth in women.3,4 HCC has a strong male predominance with male to female ratio of 2–3:1.⁵ Furthermore, HCC in non-cirrhotic patient has a bimodal presentation, peaking during the 2nd and 7th decade of life⁶ and more advance stage at the time of presentation.⁷
18-year-old teenage girl attended in our outpatient department with 4-5 months history of recurrent right hypochondriac pain and abdominal distension, swelling of feet for 1- 2 weeks. She reported loss of appetite, significant weight loss, and occasional vomiting but there were no other symptoms. There was no significant past illness, drug or family history of note. On examination, she was oriented, ill looking, anemic, icteric and bilateral pitting pedal oedema was present. Abdominal examination revealed moderate ascites with engorged blood vessel in the upper anterior and lateral abdominal wall with flow away from umbilicus. Liver is palpable liver (4 cm below the right costal margin, firm and non-tender), no splenomegaly. There were no stigmata of chronic liver disease.
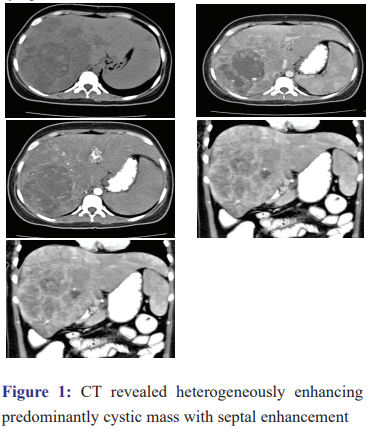
Her previous abdominal ultra-sonogram reveled multiple hyper echoic hepatic lesions with a large oval shape mixed echogenic lesion at the right lobe of liver with moderate ascites. Triphasic computed tomography (CT) was done and it revealed large heterogeneously enhancing predominantly cystic appearance mass in the right lobe of liver containing solid elements and multiple hyper dense septa. Enhancement of septa (rim enhancement around the periphery) and nodular elements are also noted. Multiple rounded enhancing nodules were noted at right lobe & left lobe of liver. Inferior vena cava was compressed by the mass and portal vein thrombosis was also noted (Fig.1). Serum alpha-fetoprotein level was 567 ng/L (normal <6 ng/L). Histopathological study of liver specimen reported atypical hepatocytes consistent with hepatocellular carcinoma (Fig. 2). CBC revealed Hb of 10.7 gm/dL, WBC of 9400/c mm, and platelets of 219,000/c mm. LFTs showed total bilirubin of 51.5 mmol/L (reference range)2-28, ALT 30 IU/L7-48, AST 4-77 U/L 7-44,alkaline phosphatase 186 U/L 32-104, Serum albumin 28 g/L 34-50. PT and PTT were normal. Serology for viral hepatitis including HBsAg, anti HBc total positive and HCV-Ab was negative. PCR for HBV-DNA was undetectable. Ascetic fluid analysis revealed no malignant cell, SAAG 1.3. Iron panel was normal. RFTs and electrolytes were normal Metastatic workup including CEA levels, CT scan of brain was normal. Chest-x-ray and chest CT scan revealed multiple nodular lesions in both lung fields. Her Child-Pugh score was 10, stage: advanced. She received only symptomatic treatment.

Cirrhosis of the liver is the single most important risk factor for HCC. In western countries, over 90% of HCC cases develop on cirrhotic individual, whereas in Asia and Africa the percentage of cases of HCC is higher in individuals with non-cirrhotic livers, compared to those with cirrhotic livers.8-9 Approximately 20% of HCC’s have been known to develop in a non-cirrhotic liver.6-10 This is consistent with our case who presented without any clinical and radiological evidence of chronic liver disease. HCC usually present at age 50-70 years. Fibro lamellar hepatocellular carcinoma (FHCC) usually occurs in young people with equal sex distribution and normal alpha fetoprotein (AFP).7 Though our patient is young, high AFP and histological findings are incongruous with the diagnosis of FHCC.
Presence of arterial enhancement of a nodule 2 cm or more in size with subsequent washout on portal or delayed phases are considered to be the definitive imaging features of HCC and recommended in the guidelines by various associations for liver studies.11,12,13 But it could present as solid, cystic or mixed lesions in the liver. Areas of necrosis or hemorrhage within the tumor create a cystic appearance on imaging.14 In case of cystic and mixed appearance arterial enhancement of septa could be differentiating feature from liver abscess. In our case, lack of systemic features, heterogeneously enhancing cystic mass with septal enhancement on CT scan, histological features are consistent with HCC.
Different modalities of treatment are available for HCC. Presence of ascites, metastasis to lungs and portal vein thrombosis precludes surgery, transplantation and trans arterial chemoembolization (TACE). Sorafenib is indicated as the first line of treatment in patients who cannot benefit from the above therapeutic options.15,16 As her Child-Pugh score was 10 and stage was advanced, she was treated symptomatically.
Although HCC is common worldwide, it is rare in teenagers and could be maiden manifestation without evidence preexisting liver disease.
The authors report no conflict of interest and no funding was received for this work.
1. Ananthakrishnan A, Gogineni V, Saeian K. Epidemiology of primary and secondary liver cancers. Semin Intervent Radiol 2006; 23: 47-63 [PMID: 21326720 DOI: 10.1055/s-2006-939841]
2. Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. CA Cancer J Clin 2005; 55: 74-108 [PMID: 15761078 DOI: 10.3322/canjclin.55.2.74]
3. Mittal S, El-Serag HB. Epidemiology of hepatocellular carcinoma: consider the population. J Clin Gastroenterol 2013; 47 Suppl: S2-S6 [PMID: 23632345 DOI: 10.1097/MCG.0b013e3182872f29]
4. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin 2018; 68: 7-30 [PMID: 29313949 DOI: 10.3322/caac.21442]
5. Bray, F. et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA. Cancer J. Clin. 68, 394–424 (2018).
6. Lee DH, Lee JM. Primary malignant tumours in the non-cirrhotic liver. Eur J Radiol 2017; 95: 349-361 [PMID: 28987692 DOI: 10.1016/j.ejrad.2017.08.030]
7. Trevisani F, Frigerio M, Santi V, Grignaschi A,Bernardi M. Hepatocellular carcinoma in non-cirrhotic liver: a reappraisal. Dig Liver Dis 2010 May;42(5):341-347.
8. Montalto G, Cervello M, Giannitrapani L, Dantona F, Terranova A, Castagnetta LA. Epidemiology, risk factors, and natural history of hepatocellular carcinoma. Ann N Y Acad Sci 2002; 963: 13-20
9. Okuda K. Hepatocellular carcinoma. J Hepatol 2000; 32: 225-237.
10. Liu S, Chan KW, Wang B, Qiao L. Fibrolamellar hepatocellular carcinoma. Am J Gastroenterol 2009; 104: 2617-24; quiz 2625 [PMID: 19638962 DOI: 10.1038/ajg.2009.440]
11. Omata M, Lesmana LA, Tateishi R, et al. Asian Pacific Association for the Study of the Liver consensus recommendations on hepatocellular carcinoma. Hepatol Int. 2010;4:439–474. doi: 10.1007/s12072-010-9165-7. . PMid:20827404
12. Bruix J, Sherman M. Practice Guidelines Committee, American Association for the Study of Liver Diseases. Management of hepatocellular carcinoma. Hepatology. 2005;42:1208–1236. doi: 10.1002/hep.20933. . PMid:16250051.
13. Forner A, Vilana R, Ayuso C, et al. Diagnosis of hepatic nodules 20 mm or smaller in cirrhosis: prospective validation of the noninvasive diagnostic criteria for hepatocellular carcinoma. Hepatology. 2008;47:97–104. doi: 10.1002/hep.21966. . PMid:18069697]
14. Bakoyiannis A, Delis S, Triantopoulou C, Dervenis C. Rare cystic liver lesions: a diagnostic and managing challenge. World J Gastroenterol. 2013;19:7603–7619. doi: 10.3748/wjg.v19.i43.7603.
15. T, Meloni F, Di Stasi M, Rolle E, Solbiati L, Tinelli C, et al. Sustained complete response and complications rates after radiofrequency ablation of very early hepatocellular carcinoma in cirrhosis: Is resection still the treatment of choice? HEPATOLOGY 2008; 47: 82-89.
16. Llovet JM, Ricci S, Mazzaferro V, Hilgard P, Gane E, Blanc JF, et al; SHARP Investigators Study Group.